New Delhi, 25 May 2025: Diabetes is a chronic condition that affects millions of people around the world, and while many associate it primarily with blood sugar control, its long-term complications can be devastating—especially for your kidneys. In fact, diabetes is the leading cause of kidney failure globally, with nearly one in three adults with diabetes suffering from some form of kidney disease. The link between high blood sugar and kidney damage is both alarming and largely under-discussed.
In this article, we explain how high blood sugar levels wreak havoc on your kidneys, the warning signs of diabetic kidney disease (DKD), and how you can protect your renal health.
How Diabetes Affects the Kidneys
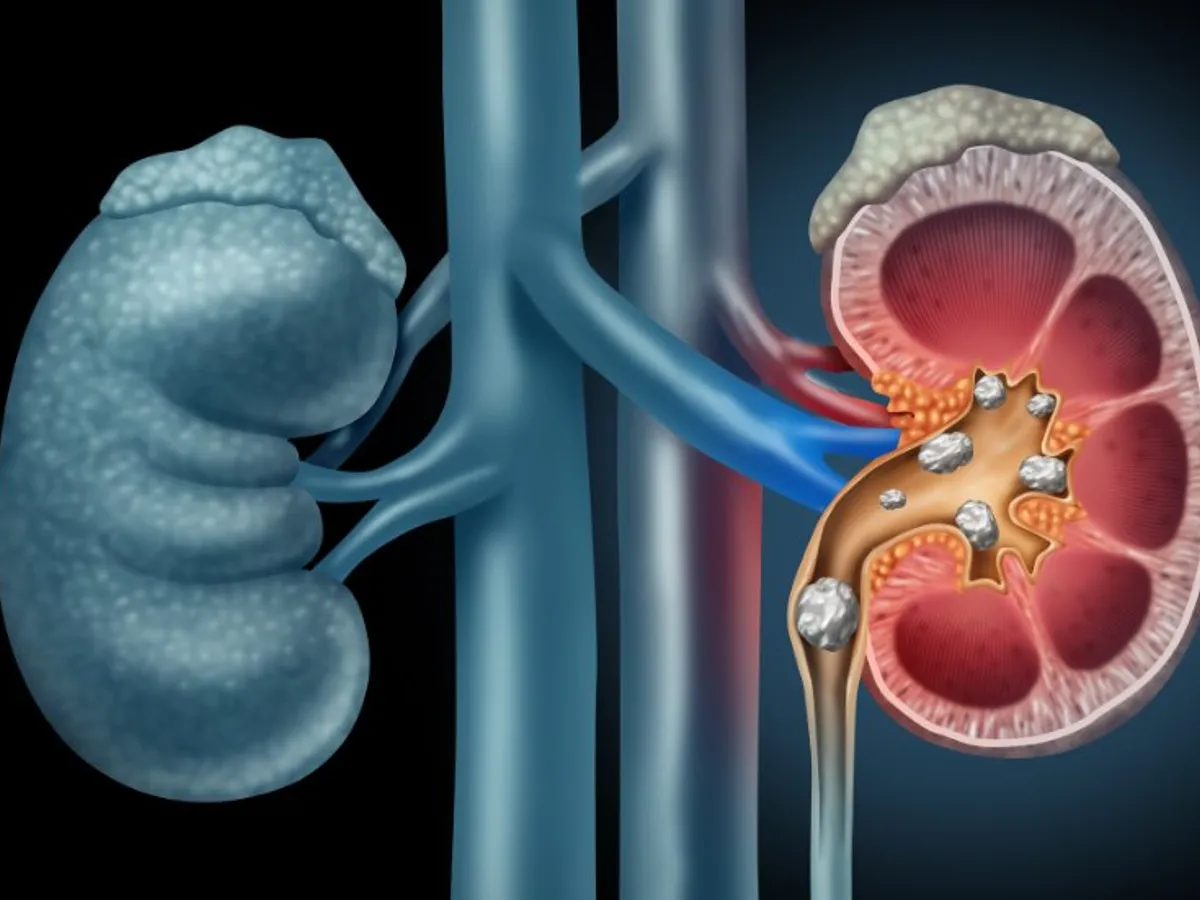
Your kidneys are responsible for filtering waste, toxins, and excess fluid from your blood through millions of tiny blood vessels called nephrons. These nephrons rely on healthy blood vessels to function efficiently. But when blood sugar levels remain elevated over long periods, they start damaging these vessels. Here’s how:
Glycation of Proteins and Vessels: High glucose levels in the blood trigger a process called glycation, where sugar molecules bind with proteins. This leads to the thickening and scarring of kidney tissues and blood vessels.
Increased Pressure in the Kidneys: Hyperglycemia (high blood sugar) also raises the pressure within the kidneys, straining the filtration system. Over time, this causes protein to leak into the urine—a sign of kidney damage.
Inflammation and Oxidative Stress: Chronic high blood sugar increases oxidative stress and inflammation, which further damages kidney tissues and accelerates the progression of kidney disease.
Stages of Diabetic Kidney Disease (DKD)
Diabetic kidney disease doesn’t happen overnight. It progresses through stages:
Stage 1: Increased kidney size and a higher glomerular filtration rate (GFR). At this point, damage is happening silently.
Stage 2: Microalbuminuria — small amounts of protein start leaking into the urine.
Stage 3: Macroalbuminuria — large protein leaks, accompanied by swelling in the legs, feet, and hands.
Stage 4: Declining GFR and rising creatinine levels — indicating significant loss of kidney function.
Stage 5: End-Stage Renal Disease (ESRD) — kidneys fail completely, requiring dialysis or a transplant.
Symptoms of Diabetic Kidney Disease
Often, early-stage kidney disease shows no symptoms, making regular screening essential for diabetics. However, as the condition progresses, the following signs may appear:
- Swelling in ankles, feet, legs, or hands
- Frequent urination, especially at night
- Blood or foam in urine
- Fatigue and weakness
- Loss of appetite and weight
- Nausea or vomiting
- Itching and dry skin
- Shortness of breath
- High blood pressure that’s hard to control
If you have diabetes and notice any of these symptoms, it’s crucial to consult a doctor immediately.
Why Blood Sugar Control Is Crucial for Kidney Health
Maintaining optimal blood glucose levels is one of the most effective ways to protect your kidneys. Studies have shown that good glycemic control can significantly slow the progression of kidney disease in diabetics.
Here’s how you can do it:
- Monitor blood sugar regularly
- Follow a diabetes-friendly diet rich in fiber, whole grains, and lean proteins, and low in salt and saturated fats
- Take medications as prescribed for both diabetes and blood pressure
- Exercise regularly to improve insulin sensitivity
- Avoid smoking and limit alcohol
- Stay hydrated, but within limits advised by your doctor if you already have kidney issues
Importance of Blood Pressure and Cholesterol Control
Besides blood sugar, high blood pressure and elevated cholesterol levels also contribute to kidney damage. People with diabetes should aim to keep their blood pressure below 130/80 mmHg. Medications like ACE inhibitors or ARBs are commonly prescribed to manage both blood pressure and kidney protection.
Can Diabetic Kidney Damage Be Reversed?
In the early stages, kidney damage can sometimes be halted or even reversed with intensive lifestyle and medical interventions. However, once the damage progresses beyond a certain point, particularly to stages 4 and 5, the condition becomes irreversible.
That said, with proper management, people with DKD can still lead a good quality of life and prevent further deterioration.
Diabetes-related kidney damage is serious, but it is not inevitable. Staying informed, getting regular check-ups, and maintaining good control over blood sugar, blood pressure, and cholesterol can make a big difference.
Kidney damage doesn’t just impair your ability to filter toxins — it can lead to life-threatening complications. Protect your kidneys the same way you protect your heart or brain: with awareness, discipline, and consistent medical care.












Leave a comment