Dr. Prerna Lakhwani Gynaecologic& Oncology, Fortis, Shalimar Bagh
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer, and can spread to other areas of the body.
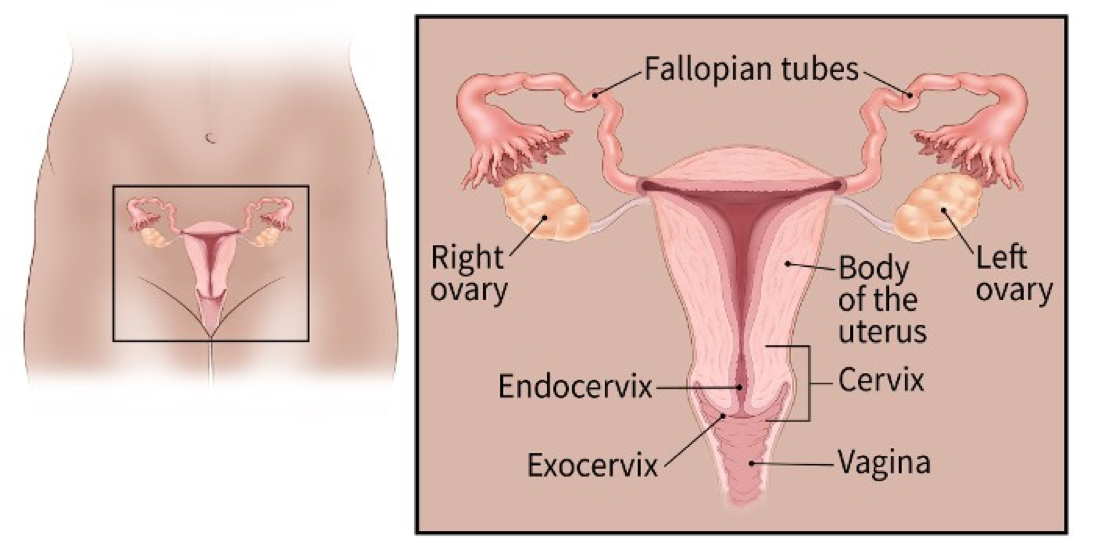
Cervical cancer starts in the cells lining the cervix — the lower part of the uterus (womb)
These cells do not suddenly change into cancer. Instead, the normal cells of the cervix first gradually develop pre-cancerous changes that turn into cancer. These changes can be detected by the Pap test and treated to prevent cancer from developing.
The best way to find cervical cancer early is to have regular screening with a Pap test (which may be combined with a test for human papilloma virus or HPV). Being alert to any signs and symptoms of cervical cancer can also help avoid unnecessary delays in diagnosis. Early detection greatly improves the chances of successful treatment and can prevent any early cervical cell changes from becoming cancerous.
Statistics for Cervical Cancer
Cancer cervix is the third most common cancer in women worldwide & second most common cancer in India. The disease is preventable by screening & early diagnosis & treatment is associated with good clinical outcome. Cervical intraepithelial neoplasia (CIN) is the premalignant stage of disease & Human papilloma virus (HPV) is identified as causative agent in most cases.
Cervical cancer constitutes 13% of all cancers in women globally. It was the most common cancer in India until a few years ago. The 2008 estimates in India are 134,420 cases annually with 72,425 deaths occurring due to it bringing out the incidence rate to ~23.5/100,000 women.
International data show a decline in incidence of cervical cancer in countries with successful screening program & early intervention. A decrease is also noted in India & now breast cancer tops the list of female cancers followed closely by cervical cancer.
Vaccines to prevent cervical cancer
Human papillomavirus (HPV) has been found to be the primary cause of cervical cancer, associated with nearly all cervical malignancies. Of more than 100 HPV types, about 15 are found to be high-risk with the potential to cause cancer. HPV is a common sexually transmitted infection. Though the majority of HPV infections are asymptomatic and resolve spontaneously, persistent infection with high-risk HPV types, in the presence of co-factors, can lead to the development of pre-cancerous cervical lesions, cervical cancer, and other cancers including vaginal and vulvar cancers in women; penile cancer in men; and anal and oropharyngeal cancers in both men and women.
The two HPV vaccines currently available in India – bivalent (Cervarix®, GlaxoSmithKline) and quadrivalent (Gardasil®, Merck& Co.Inc.) – have demonstrated high efficacy in clinical trials. The efficacy of the vaccines is almost 100% against persistent cervical infection and pre-cancerous cervical lesions associated with HPV types 16 and 18 in girls/women who are free from HPV infection at baseline. In light of strong evidence, Asian countries such as Bhutan, Malaysia, Philippines, Brunei, Laos, Nepal, Bangladesh and Sri Lanka have introduced the HPV vaccine in their national immunization programs.
The World Health Organization (WHO) recommends that adolescent girls 9–13 years of age be vaccinated because the vaccine is highly immunogenic at this age and girls are typically not yet exposed to the virus. The recently published results of a study from India that administered approximately 35,000 doses in girls 10-18 years of age with a 4-year follow- up reported no serious adverse events attributable to the HPV vaccine. Even after nearly 10 years of use there is no evidence of waning vaccine effectiveness have been reported. Regardless of HPV vaccination status, cancer screening by Pap test, visual inspection with acetic acid (VIA) and/or HPV testing are also recommended as the vaccine does not protect against all high risk HPV types. The HPV vaccine can actually help protect fertility by preventing gynecological problems related to the treatment of cervical cancer and pre-cancerous lesions















Leave a comment