New Delhi, 18 September, 2025: Kerala is once again grappling with the alarming spread of a rare but deadly infection caused by the brain-eating amoeba, Naegleria fowleri. This microscopic organism has claimed 19 lives so far, sparking fears among residents and health authorities. Known for its extremely high fatality rate, this amoeba thrives in warm freshwater sources and enters the human body through the nose, eventually causing a brain infection called Primary Amoebic Meningoencephalitis (PAM).
Although such infections are rare, their rapid progression and high mortality make them a major public health concern. Let’s understand what this amoeba is, how it spreads, its symptoms, and what you can do to stay safe.
What is the Brain-Eating Amoeba?
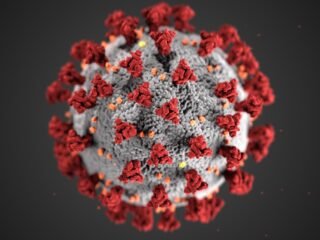
The brain-eating amoeba, Naegleria fowleri, is a free-living microorganism found in warm freshwater bodies such as lakes, rivers, ponds, and poorly maintained swimming pools. Contrary to its terrifying nickname, the amoeba does not “eat” brain tissue directly. Instead, once it enters the nasal passages, it travels along the olfactory nerve to the brain, causing severe inflammation and damage.
The condition it triggers — Primary Amoebic Meningoencephalitis (PAM) — is extremely aggressive, with survival rates as low as 3-5% globally.
How Does the Infection Spread?
The amoeba does not spread from person to person. Instead, infection occurs when contaminated water enters the nose.
Common situations where infection risk is higher include:
- Swimming or diving in untreated freshwater bodies during hot weather.
- Using contaminated tap water for nasal rinsing (e.g., during religious or cleaning practices).
- Exposure to poorly chlorinated swimming pools or hot springs.
- Using stagnant or unfiltered water in households.
Once inside the nose, the amoeba travels quickly to the brain, often causing death within days.
Symptoms of Brain-Eating Amoeba Infection
The first symptoms usually appear 1–9 days after exposure, but the illness worsens rapidly.
Early symptoms may mimic meningitis, making it difficult to diagnose immediately:
- Severe headache
- Fever
- Nausea and vomiting
- Stiff neck
As the infection progresses, more alarming symptoms develop:
- Confusion and disorientation
- Seizures
- Loss of balance
- Hallucinations
- Coma
Most patients die within 5–12 days of symptom onset.
Why Kerala Is Facing a Rising Threat
Kerala has witnessed increasing cases of Naegleria fowleri infections, with climate change and rising temperatures being major contributors. Warm, stagnant water bodies create the perfect breeding ground for the amoeba.
Experts also warn that:
- Poor water management in rural areas increases contamination risk.
- Changing weather patterns have expanded the amoeba’s presence in regions previously considered safe.
- Religious practices involving nasal cleansing with untreated water may unknowingly increase exposure.
This year’s outbreak highlights how a mix of environmental and lifestyle factors can make even rare pathogens a recurring public health concern.
Dos and Don’ts to Stay Safe
Since there is no guaranteed cure for brain-eating amoeba infections, prevention is the best defense. Here are essential Dos and Don’ts:
Dos:
- Use clean, treated, or boiled water for nasal rinsing, drinking, or cleaning.
- Wear nose clips while swimming or diving in freshwater bodies.
- Ensure swimming pools are properly chlorinated and well-maintained.
- Seek immediate medical care if you experience sudden high fever, severe headache, or confusion after water exposure.
- Stay updated with health advisories in outbreak-prone regions.
Don’ts:
- Do not swim or dive in stagnant, untreated, or warm freshwater lakes, ponds, or rivers.
- Do not use tap water for nasal cleansing unless it is boiled and cooled.
- Do not neglect early flu-like symptoms after water activities.
- Do not assume all water sources are safe — always check treatment and cleanliness.
Can the Infection Be Treated?
Treatment options for PAM are very limited and often unsuccessful. Doctors may try combinations of antifungal and antimicrobial drugs such as amphotericin B, rifampicin, and miltefosine, but the survival rate remains dismally low.
Early diagnosis is critical, but unfortunately, most cases are detected late due to symptom similarity with meningitis or viral infections.
Expert Warnings
Medical experts caution that Kerala’s outbreak is a wake-up call for both citizens and health authorities. Climate change is altering the ecology of pathogens, making rare infections more frequent. Public awareness, improved water safety, and better diagnostic preparedness are essential to save lives.
An infectious disease specialist, noted: “People should understand that prevention is the only effective strategy against Naegleria fowleri. Once symptoms appear, the chances of survival are extremely slim.”
The tragic deaths of 19 individuals in Kerala from brain-eating amoeba infections underline the urgency of vigilance. While the disease remains rare, its deadliness and rapid progression mean prevention cannot be ignored.
By following simple hygiene practices, avoiding risky water exposure, and seeking immediate medical help when symptoms occur, people can greatly reduce the threat.
As climate and environmental conditions evolve, awareness and proactive measures will be the strongest shields against such deadly pathogens.














Leave a comment