New Delhi, 03 November, 2025: The kidneys are remarkable organs that quietly perform some of the most vital functions in our body — filtering waste, balancing fluids and electrolytes, regulating blood pressure, and even producing hormones that control red blood cell production. However, when blood pressure or blood sugar levels rise beyond the normal range, the kidneys can become one of the first organs to suffer silent but serious damage.
In this article, we’ll explore in depth how high blood pressure (hypertension) and high blood sugar (hyperglycemia) affect kidney function, why these conditions are often linked, and how you can protect your kidneys for life.
Understanding Kidney Function
Each kidney contains about one million tiny filtering units called nephrons. These nephrons consist of glomeruli — networks of small blood vessels (capillaries) — and tubules that help remove waste and excess fluids from the bloodstream.
Healthy kidneys filter about 180 liters of blood daily, excreting toxins and waste through urine while keeping essential proteins and cells in the bloodstream.
When the blood supply to these delicate filters is compromised — whether by high blood pressure or high blood sugar — the filtration system becomes damaged over time, leading to chronic kidney disease (CKD).
How High Blood Pressure Damages the Kidneys
High blood pressure (BP) means the force of blood against your artery walls is consistently too strong. Over time, this pressure can cause arteries throughout the body, including those in the kidneys, to weaken, narrow, or harden.
1. Damage to Renal Blood Vessels
The kidneys depend on a rich network of tiny blood vessels to perform filtration. When blood pressure is too high, these vessels stretch and thicken in an attempt to withstand the force. This leads to arteriosclerosis (hardening of the arteries) and reduced blood flow to the nephrons.
As a result, less oxygen and nutrients reach kidney tissues, impairing their ability to filter blood efficiently.
2. Glomerular Hypertension and Hyperfiltration
In the early stages of high blood pressure, the kidneys may try to compensate by increasing filtration pressure. This “hyperfiltration” phase might seem like the kidneys are working harder, but over time, the excessive pressure within glomeruli leads to glomerulosclerosis — scarring of the filtering units.
Once these glomeruli are damaged, they can’t regenerate, leading to permanent loss of kidney function.
3. Sodium and Fluid Retention
Damaged kidneys struggle to excrete sodium effectively. The buildup of sodium causes the body to retain water, further increasing blood pressure — creating a vicious cycle known as the hypertension-kidney disease loop.
4. Silent Progression
High BP–induced kidney damage often progresses without symptoms until kidney function is severely impaired. Early indicators include microalbuminuria, where small amounts of protein leak into the urine — a sign that the glomeruli are starting to fail.
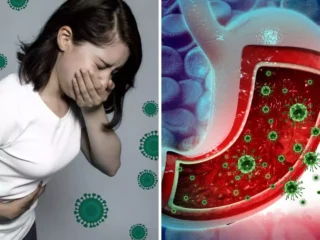
How High Blood Sugar Harms the Kidneys
Diabetes — both Type 1 and Type 2 — is the leading cause of kidney failure worldwide. The kidneys play a central role in filtering glucose from the bloodstream. When blood sugar levels remain elevated for prolonged periods, this delicate filtration system suffers extensive wear and tear.
1. Glucose Toxicity and Glycation
Excess glucose in the blood reacts with proteins and lipids, forming harmful compounds known as advanced glycation end-products (AGEs). These AGEs damage kidney cells and the glomerular basement membrane, making it thicker and less permeable — a hallmark of diabetic nephropathy.
2. Hyperfiltration in Early Diabetes
In the early stages of diabetes, the kidneys often work overtime to filter the excess glucose — leading again to glomerular hyperfiltration. While initially compensatory, this overactivity gradually damages the glomeruli, setting the stage for chronic kidney disease.
3. Oxidative Stress and Inflammation
Persistently high glucose levels generate free radicals (oxidative stress), which inflame and scar kidney tissue. The body’s inflammatory response leads to fibrosis — a thickening and stiffening of the kidney’s internal structures — reducing filtration efficiency.
4. Protein Leakage and Kidney Scarring
As glomeruli become damaged, essential proteins such as albumin begin leaking into the urine. This condition, known as proteinuria, accelerates kidney scarring and reduces their filtering capacity further.
Why High BP and High Blood Sugar Often Occur Together
Hypertension and diabetes often coexist — and when they do, the risk of kidney damage multiplies.
- Insulin resistance, a hallmark of Type 2 diabetes, can lead to both elevated blood sugar and increased sympathetic nervous system activity, which raises blood pressure.
- High blood pressure, in turn, worsens insulin resistance, making glucose control harder.
- Over time, both conditions damage blood vessels throughout the body — especially the microvessels in the kidneys.
This dangerous combination is often referred to as the “deadly duo” for kidney health.
The Stages of Diabetic and Hypertensive Kidney Disease
Kidney damage from diabetes or hypertension progresses through several stages:
- Hyperfiltration Stage: Increased kidney workload; no symptoms yet.
- Microalbuminuria: Small amounts of protein appear in urine.
- Macroalbuminuria: Protein levels rise; kidney filtering efficiency declines.
- Chronic Kidney Disease (CKD): Waste accumulates; blood pressure and electrolyte imbalances worsen.
- End-Stage Renal Disease (ESRD): Kidneys fail; dialysis or transplantation becomes necessary.
Symptoms to Watch For
Kidney disease develops slowly and silently. However, some warning signs include:
- Swelling in the feet, ankles, or around the eyes
- Fatigue or weakness
- Changes in urination (frequency, color, or foaming)
- Persistent high blood pressure
- Nausea, vomiting, or loss of appetite
- Unexplained shortness of breath (due to fluid retention)
If you have diabetes or hypertension, routine kidney function tests — such as eGFR (estimated glomerular filtration rate) and urine albumin-to-creatinine ratio (UACR) — are crucial for early detection.
Preventing Kidney Damage: What an Endocrinologist Recommends
1. Keep Blood Sugar Under Control
Maintaining near-normal glucose levels is the single most important step in preventing diabetic kidney disease.
- Target HbA1c: Ideally below 7%, though individualized goals may vary.
- Monitor regularly: Frequent glucose monitoring helps detect trends early.
- Medication: Metformin, SGLT2 inhibitors, and GLP-1 receptor agonists have shown benefits for both blood sugar control and kidney protection.
- Diet: Reduce simple sugars and refined carbs; focus on high-fiber foods, vegetables, and lean proteins.
2. Manage Blood Pressure Aggressively
- Target BP: Less than 130/80 mmHg for most patients with diabetes or CKD.
- Medications: ACE inhibitors and ARBs not only lower blood pressure but also protect glomeruli by reducing intraglomerular pressure.
- Salt restriction: Aim for less than 2 grams of sodium per day (around 5 grams of salt).
- Physical activity: At least 30 minutes of moderate exercise 5 days a week helps lower BP naturally.
3. Maintain a Healthy Weight
Excess body fat contributes to both insulin resistance and elevated blood pressure. Even a 5–10% reduction in body weight can significantly improve kidney and cardiovascular outcomes.
4. Stay Hydrated — But Smartly
While adequate hydration is essential, those with advanced kidney disease may need to limit fluids. Always follow your doctor’s advice regarding daily water intake.
5. Avoid Nephrotoxic Substances
Certain painkillers (like NSAIDs), contrast dyes, and herbal supplements can strain the kidneys further. Consult your doctor before taking any new medication or supplement.
6. Stop Smoking and Limit Alcohol
Smoking constricts blood vessels and worsens both hypertension and diabetes. Alcohol adds extra calories and may interfere with blood pressure and glucose medications.
The Importance of Regular Screening
Both diabetes and hypertension can damage kidneys long before symptoms appear. That’s why endocrinologists emphasize preventive screening:
- Annual eGFR and urine microalbumin tests for all patients with diabetes or hypertension.
- Comprehensive metabolic panels to monitor electrolyte balance and kidney function.
- Eye and heart exams, since microvascular damage often affects multiple organs simultaneously.
When to See a Nephrologist
If lab results show declining kidney function (eGFR < 60 mL/min/1.73 m² or persistent proteinuria), your endocrinologist may refer you to a nephrologist — a kidney specialist — for co-management. Early collaboration between specialists can slow or even halt disease progression.
High blood pressure and high blood sugar are two of the leading — and most preventable — causes of kidney disease. Their effects are cumulative, progressive, and often silent. But the good news is that early detection, disciplined control, and lifestyle management can dramatically reduce your risk.