New Delhi: Every year, World Kidney Day serves as a reminder of the importance of kidney health in global wellbeing. Yet one of the most vital—but often misunderstood—messages of this observance is that kidney health cannot be discussed in isolation. The kidneys and the heart are deeply interconnected. When one weakens, the other is almost always affected. Today, as chronic disease rates rise worldwide, understanding this two-way relationship between the heart and kidneys has never been more critical.
The interplay between these organs is not a simple partnership—it is a complex physiological dialogue. Their relationship is constant and reciprocal: the heart pumps blood to supply the kidneys, and the kidneys regulate blood pressure, fluid levels, and electrolyte balance to ensure the heart can function optimally. When that dialogue breaks down, the consequences can be life-altering. Heart failure can accelerate kidney failure, and kidney decline can trigger cardiovascular disease. For millions of people, this “cardiorenal connection” quietly shapes health outcomes long before symptoms arise.
Why the Heart and Kidneys Are Inseparable Partners
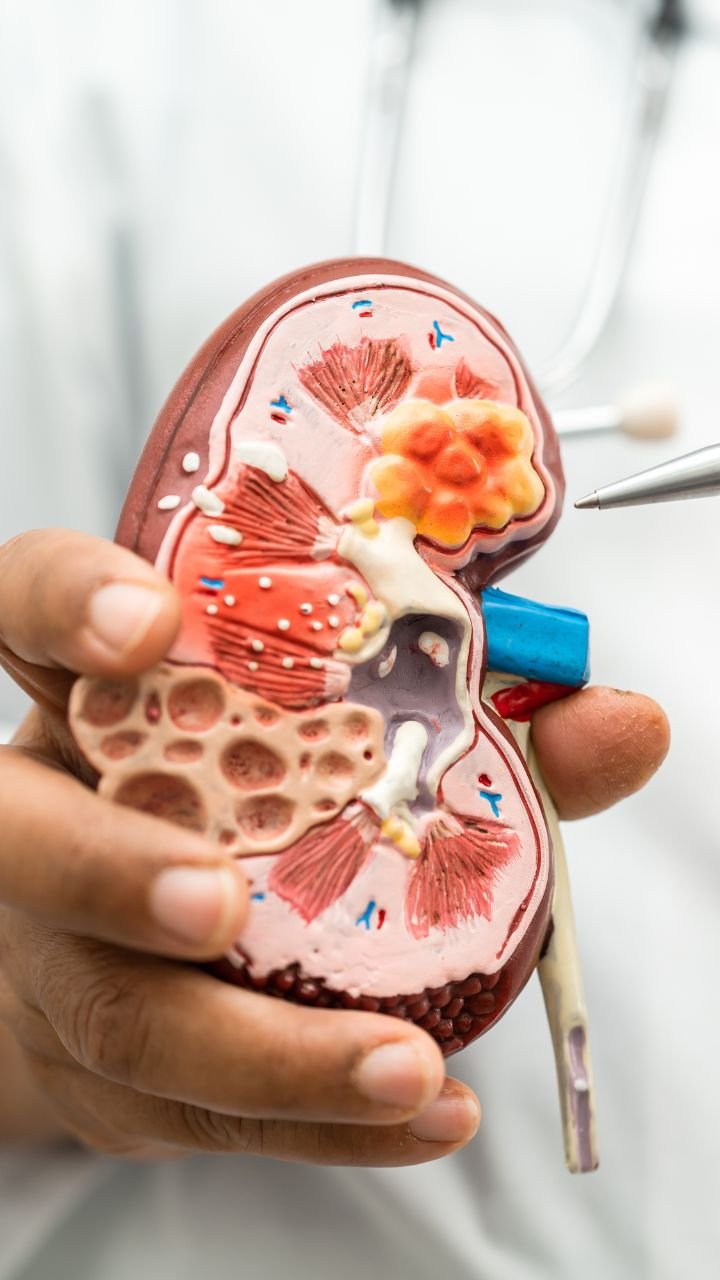
To appreciate the significance of this relationship, it helps to understand the core roles each organ plays.
The Heart: The Engine That Keeps Kidneys Working
The kidneys receive roughly 20% of the body’s blood output—more than almost any other organ. This constant high-volume supply allows them to filter waste, maintain fluid balance, and regulate key hormones. If the heart’s pumping ability declines, whether from heart failure, heart attack, or chronic high blood pressure, the kidneys receive less blood. Reduced blood flow starves their tissues of oxygen and nutrients, eventually impairing filtration.
The Kidneys: The Regulators of Heart Health
The kidneys influence cardiovascular function through several vital mechanisms:
- Regulating blood pressure via fluid and electrolyte balance
- Producing hormones that affect blood vessel tone
- Managing sodium levels, which directly influence blood pressure
- Controlling acid-base balance, crucial for heart function
- Producing erythropoietin, which affects red blood cell production and oxygen delivery
When kidney function declines—even slightly—these regulatory systems begin to falter. Blood pressure rises, fluid overload occurs, and toxins accumulate—all of which place immense strain on the heart.
Thus, the relationship is inherently circular: heart problems worsen kidney function, and kidney problems worsen heart function.
The Silent Nature of Cardiorenal Disease
One of the biggest challenges is that early damage to either organ often develops slowly and without obvious symptoms. Many people have mild to moderate kidney impairment or subtle heart dysfunction without realizing it.
By the time symptoms appear—swelling, shortness of breath, fatigue, irregular heart rhythms—significant organ damage may already be present. This delay in detection is one reason cardiovascular disease is more deadly in people with kidney impairment and, conversely, why kidney disease is more likely in individuals with heart failure.
How Kidney Disease Raises Heart Risk
Research over the past decade has made it clear that even minor reductions in kidney function significantly increase the risk of cardiovascular disease.
Several mechanisms explain why:
1. High Blood Pressure
As kidneys lose their filtering ability, excess sodium and fluid accumulate. This raises blood volume and blood pressure, increasing strain on the heart and blood vessels.
2. Vascular Calcification
Impaired kidneys disrupt calcium and phosphorus balance, leading to the buildup of calcium in arteries. This stiffens blood vessels, making them less able to handle fluctuations in pressure and increasing the risk of heart attacks and strokes.
3. Chronic Inflammation
Kidney impairment triggers inflammation throughout the body, accelerating atherosclerosis (plaque buildup in arteries).
4. Anemia
Reduced production of erythropoietin leads to anemia, forcing the heart to work harder to supply oxygen to tissues.
5. Fluid Overload
When kidneys can’t excrete fluid effectively, the resulting volume overload puts additional stress on the heart’s pumping ability.
These interconnected pathways explain why people with chronic kidney disease are far more likely to die from heart disease than from kidney failure itself.
How Heart Disease Damages the Kidneys
The relationship is equally strong in the opposite direction. Any condition that weakens the heart can reduce the blood flow that kidneys depend on.
1. Heart Failure
As the heart becomes less effective at pumping, the kidneys receive inadequate blood flow. This activates hormonal systems—particularly the renin–angiotensin–aldosterone system—that initially try to compensate but ultimately worsen both heart and kidney function.
2. Reduced Cardiac Output
Following heart attacks or in conditions such as cardiomyopathy, the heart may not generate enough pressure to sustain kidney filtration. Over time, this leads to structural kidney damage.
3. Chronic High Blood Pressure
Hypertension damages blood vessels throughout the body, including the delicate vessels in the kidneys. This damage is a major driver of long-term kidney decline.
4. Medications Used in Heart Disease
Certain heart medications can inadvertently harm the kidneys, particularly if doses are not carefully adjusted. This makes collaborative care essential.
This pattern, in which heart dysfunction leads to kidney damage, is often referred to as cardiorenal syndrome, highlighting the intertwined nature of the two systems.
Why This Relationship Is a Global Public Health Issue
As populations age and rates of diabetes, hypertension, and obesity rise, both heart and kidney diseases are becoming more prevalent worldwide. The fact that these conditions so often coexist compounds their individual burdens.
Several trends amplify the urgency:
- Increasing global prevalence of hypertension
- Surging rates of chronic kidney disease, especially in developing countries
- Environmental stressors such as pollution and heat exposure
- Limited access to early screening in many regions
- Rising rates of heart failure
Because of their two-way relationship, heart and kidney diseases act as “force multipliers” for each other, accelerating disability, hospitalization, economic costs, and premature death.
The Need for Collaboration Between Specialties
One of the most important lessons emerging from the cardiorenal connection is the need for closer collaboration between cardiologists and nephrologists. Historically, heart disease and kidney disease were treated in silos. But today, integrated care is essential.
Examples include:
- Shared treatment plans for managing fluid balance
- Coordinated medication strategies to reduce harm to both organs
- Early referral to nephrology for heart failure patients
- Blood pressure targets designed to protect both heart and kidneys
- Combined clinics specializing in cardiorenal management
Integrated care improves outcomes, reduces hospitalizations, and helps identify problems earlier.
What Individuals Can Do to Protect Both Heart and Kidney Health
The steps to protect your kidneys and heart are remarkably similar. They revolve around managing risk factors and making long-term lifestyle changes.
1. Monitor Blood Pressure
High blood pressure is one of the strongest threats to both organs. Regular monitoring and treatment are essential.
2. Manage Blood Sugar
Diabetes is a leading cause of CKD and significantly increases heart disease risk.
3. Maintain a Healthy Weight
Even modest weight loss can reduce strain on both systems.
4. Exercise Regularly
Physical activity improves circulation, supports kidney function, and lowers cardiovascular risk.
5. Follow a Heart- and Kidney-Friendly Diet
This includes limiting sodium, reducing ultra-processed foods, increasing fruits and vegetables, and moderating protein intake when kidney function is impaired.
6. Avoid Smoking
Smoking accelerates both vascular disease and kidney decline.
7. Get Regular Screening
Simple blood and urine tests can identify early kidney dysfunction long before symptoms appear.
A Shared Future for Heart and Kidney Health
This World Kidney Day, it’s essential to bring renewed attention to a truth too often overlooked: heart health and kidney health are inseparable. What affects one will inevitably affect the other. Recognizing their two-way relationship is more than a medical insight—it is a call to action for health systems, policymakers, clinicians, and individuals.
By understanding the profound connection between these two vital organs and acting early to protect them, we have an opportunity to reduce the burden of chronic disease worldwide, prevent avoidable deaths, and empower people to lead longer, healthier lives.