New Delhi, 13 August 2025: In the realm of rare diseases, few are as devastating and challenging as Spinal Muscular Atrophy (SMA). This genetic neuromuscular disorder leads to the progressive weakening of muscles and, without timely treatment, can be fatal—particularly in children. With treatment costs soaring as high as ₹16 crore for a single injection, SMA presents not only a medical challenge but also an emotional and financial burden for affected families.
In this section, Dr. Shankaracharya, Chairperson, Spine Surgery Department, Sir Ganga Ram Hospital, Tells us more about this genetic neuromuscular disorder.
Let’s begin by understanding — what exactly is Spinal Muscular Atrophy (SMA), and why is it considered such a rare and critical disorder?
What Is Spinal Muscular Atrophy (SMA)
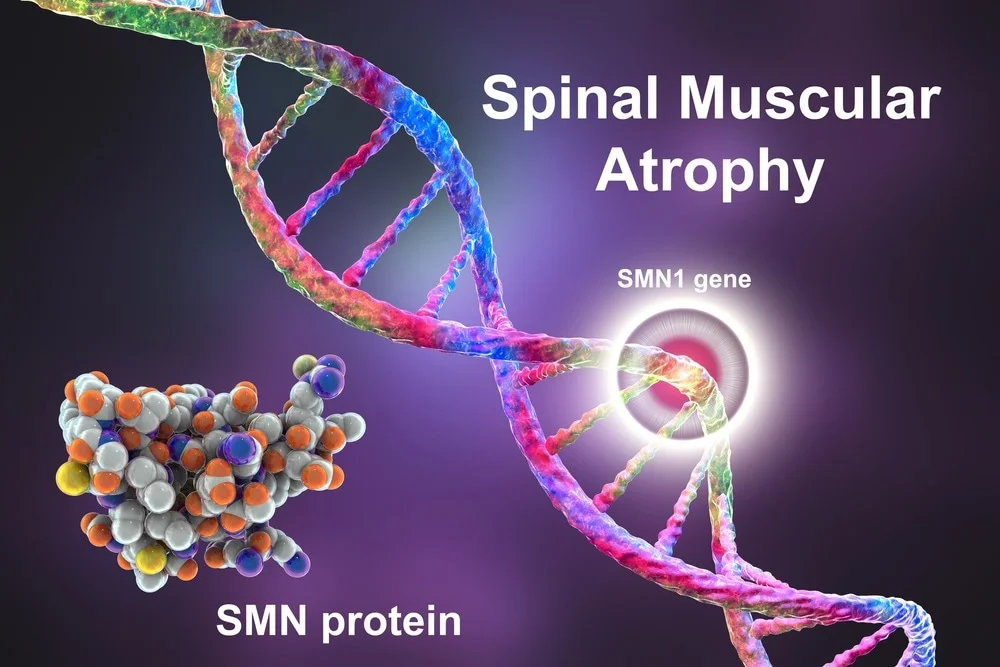
Dr. Shankaracharya: Spinal Muscular Atrophy, or SMA, is a rare genetic disorder that affects the motor neurons — the nerve cells in the spinal cord responsible for muscle movement. It’s classified as an autosomal recessive condition, which means that both parents must carry the defective gene for a child to be affected. The disease is caused by a deletion in the SMN1 gene, leading to a deficiency of the SMN protein necessary for motor neuron survival. Without it, these neurons degenerate, causing progressive muscle weakness and, in severe cases, death.
Is it true that a single injection used in its treatment costs ₹16 crore?
Dr. Shankaracharya: Yes, that’s correct. The most advanced treatment available is gene therapy, specifically the drug Zolgensma, which is administered as a single injection and costs around ₹16 crore. It’s currently one of the most expensive drugs in the world because it’s patented, cutting-edge, and involves highly complex gene replacement technology. We use a viral vector (adenovirus) to insert a healthy copy of the SMN1 gene into the patient’s body, allowing it to produce the missing protein.
Why is this treatment so expensive, and are there any affordable alternatives available in India?
Dr. Shankaracharya: The high cost is primarily due to monopoly patents, the complexity of production, and regulatory pathways. That said, India does have more affordable options, such as oral or injectable drugs developed by Natco Pharma, which cost around ₹75,000–₹80,000. These drugs target the SMN2 gene — a backup copy of SMN1 — to enhance protein production, though they’re less effective than gene therapy. Supportive treatments like physiotherapy, respiratory care, bracing, and spinal surgeries also play a vital role.
Is SMA always present from birth, or can it develop later?
Dr. Shankaracharya: SMA is present from birth. The symptoms may appear at different ages, depending on the type — from infancy (Type 1) to adulthood (Type 4). The earliest and most severe form manifests in the first six months of life. Without treatment, these children typically do not survive beyond two years. However, late-onset SMA may allow children to walk or sit before symptoms progress.
What are the early warning signs that parents should look out for?
Dr. Shankaracharya: Parents should watch for delayed motor milestones — if the baby isn’t holding their head by 6 months, sitting by 9 months, or walking by 12 months, it could be a red flag. Floppiness, weak cry, poor sucking or swallowing, and difficulty breathing are also signs. The condition is often referred to as “Floppy Baby Syndrome” in severe cases. Spinal curvature, dislocated hips, and muscle thinning are also common as the disease progresses.
How is SMA diagnosed? Can it be identified at birth?
Dr. Shankaracharya: While SMA can’t usually be diagnosed immediately after birth without specific screening, it becomes evident through delayed development. Once symptoms appear, genetic testing is the gold standard. Other tests like muscle biopsy or blood enzyme levels (e.g., creatine kinase) can support diagnosis. We recommend genetic counseling, especially in families with a history or those from regions where consanguineous marriages are more common, which increases the risk of recessive genetic disorders.
Are treatments accessible for families who can’t afford the gene therapy?
Dr. Shankaracharya: Yes, and this is an important point. Crowdfunding, government schemes, and support from the Supreme Court and Ministry of Health are helping families access treatment. In fact, our hospital has a dedicated genetic medicine unit, and we collaborate with support groups, pediatricians, and physiotherapists to provide comprehensive care. Some patients are also on oral alternatives that are more affordable and still help manage the disease. In some cases, children have survived into adulthood with the right care and alternative therapies.
Is it fair to say that early intervention can change the outcome?
Dr. Shankaracharya: Absolutely. Early diagnosis and timely treatment can significantly improve quality of life and survival. Even if gene therapy isn’t accessible, physiotherapy, assisted breathing, nutrition, and medication can extend life and improve functionality. We’ve seen children live well into their 20s, even undergoing spinal surgeries, thanks to committed care from families and healthcare providers.
Lastly, are there any recent breakthroughs in SMA treatment that give families more hope?
Dr. Shankaracharya: Yes, there’s tremendous progress. From no treatment a decade ago, we now have gene therapy, RNA-modifying drugs, and early diagnostic tools. The concept of gene replacement was science fiction not long ago — now it’s reality. And we are hopeful that with time, costs will come down, making these life-saving treatments more accessible to all.
SMA may be a rare disease, but with advances in gene therapy, increased awareness, and multidisciplinary care, it is no longer a hopeless condition. Families need not suffer in silence. There is help, there is hope, and most importantly — there is life beyond the diagnosis.