New Delhi, 06 October, 2025: India has opened a criminal investigation into the tragic deaths of at least ten children allegedly caused by a contaminated cough syrup. The move marks one of the strongest actions yet in a series of safety crises that have shaken confidence in the country’s pharmaceutical sector.
Authorities say preliminary lab tests found that the syrup contained toxic levels of an industrial chemical — a discovery that has triggered nationwide outrage, regulatory crackdowns, and questions about how such a deadly product reached the market.
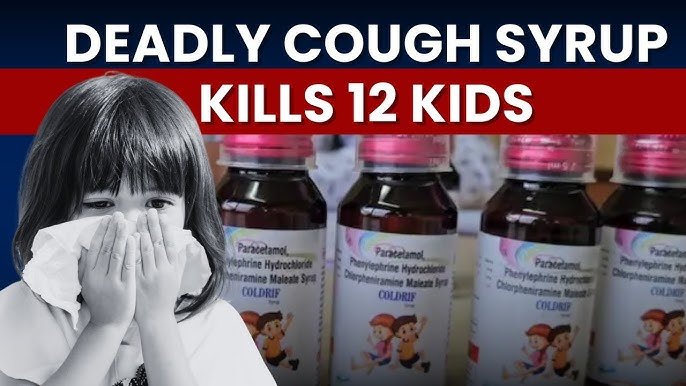
India Launches Criminal Case Over Cough Syrup Linked to Deaths of 10 Children
Police in Tamil Nadu have registered a case against Sresan Pharma, the manufacturer of the cough syrup, and a doctor who allegedly prescribed it to several children who later died. The charges include drug adulteration, negligence, and possible culpable homicide not amounting to murder.
Investigators believe the syrup’s formulation contained diethylene glycol (DEG) — a clear, sweet-tasting solvent often used in industrial applications such as brake fluid or antifreeze. When ingested, DEG can destroy the kidneys and nervous system, leading to organ failure and death.
The doctor involved, identified as Dr. Praveen Soni, was based in Parasia, Chhindwara district, Madhya Pradesh, where most of the deaths occurred. He has since been suspended from duty, and his clinic has been sealed pending investigation. State health officials say the children developed symptoms such as vomiting, decreased urine output, and lethargy — classic indicators of toxic poisoning — after being given the syrup for common colds and coughs.
The Cough Syrup in Question
The product at the center of the case is Coldrif Cough Syrup, manufactured by Sresan Pharma in Tamil Nadu’s Kanchipuram district. Lab tests reportedly revealed an alarming concentration of diethylene glycol — almost fifty times the permissible limit.
Health authorities have now classified the batch as “Not of Standard Quality” and ordered an immediate statewide ban on its sale and distribution. Pharmacies have been instructed to pull all remaining bottles off the shelves, and samples from other batches have been sent for re-testing.
According to investigators, the contaminated batch had been distributed to local clinics and pharmacies across parts of Madhya Pradesh. The children who died were all from poor families who sought basic treatment for seasonal infections. When the syrup made them sicker, most parents struggled to find dialysis facilities in the small town of Parasia and had to travel nearly 150 kilometers to Nagpur for treatment. Several children did not survive the journey.
For the families of the victims, the tragedy has left wounds that no investigation can heal. Parents describe how their children, many under five years old, went from mild coughs to kidney failure within days. Some families sold jewelry or borrowed money to pay for treatment. Others could only watch helplessly as their children deteriorated.
In Parasia, many hospitals lack advanced medical facilities such as pediatric dialysis units. This lack of critical care infrastructure compounded the crisis and has become a flashpoint for local anger. Villagers have since demanded stronger public health systems and accountability for the officials who allowed a substandard drug to circulate unchecked.
The state government has announced compensation for the affected families, but parents insist that justice will only be served when those responsible — from the manufacturers to the regulators — face punishment.
Coldrif Cough Syrup Kills Kids: How Contamination Happens
Experts say such tragedies are usually preventable. In legitimate pharmaceutical manufacturing, ingredients like glycerin or propylene glycol are used as safe solvents in syrups. However, in cases of cost-cutting or negligence, these can be substituted with cheaper industrial chemicals like diethylene glycol or ethylene glycol.
These substances are highly toxic to humans but can be difficult to detect without proper quality control. Once ingested, DEG is metabolized into harmful compounds that cause acute kidney injury, neurological damage, and metabolic acidosis. Even small doses can be fatal to children.
This kind of contamination has a deadly history. Similar poisoning cases have been reported in several countries, including The Gambia and Uzbekistan, where Indian-made syrups were implicated in dozens of child deaths. Each incident prompted international scrutiny but only limited regulatory reform.
Government and Regulatory Response
The Indian government has responded with a flurry of actions. The Madhya Pradesh health department has imposed a full ban on Coldrif syrup, and police raids have been conducted at Sresan Pharma’s facility in Tamil Nadu. Samples from multiple production batches have been seized for further testing.
Meanwhile, the Union Health Ministry has directed all state drug controllers to conduct immediate inspections of cough syrup manufacturers and test products currently in circulation. A special task force has been formed to review the regulatory framework governing over-the-counter medicines for children.
In addition, state governments across India have begun taking preventive steps. Kerala has restricted the sale of all cough syrups without prescription. Uttar Pradesh has ordered a statewide drive to test samples from pharmacies and wholesalers. Maharashtra, too, has issued an emergency order banning Coldrif syrup after confirming the presence of industrial solvents.
The central government has reportedly recommended the cancellation of Sresan Pharma’s manufacturing license and initiated legal proceedings against company executives. Officials have emphasized that the crackdown is intended not only to punish negligence but also to send a message across the pharmaceutical industry that public safety cannot be compromised.
The tragedy exposes deeper cracks in India’s drug regulation and quality control systems. India is one of the world’s largest producers of generic medicines, supplying nearly half of the pharmaceuticals used in developing countries. Yet oversight at the domestic level often remains inconsistent.
Periodic inspections in recent years have revealed that dozens of small and mid-sized drug manufacturers failed to comply with basic Good Manufacturing Practices. In some cases, facilities lacked proper documentation, equipment maintenance, or testing records. Despite this, many continued to operate with minimal penalties.
Public health experts argue that this lax enforcement allows low-quality products to enter the market, putting millions at risk. They also point to the need for better coordination between state and central drug authorities, stronger supply chain audits, and the use of advanced analytical technology to detect contamination early.
The Coldrif case also has international implications. In recent years, several countries have expressed concern about the safety of Indian pharmaceutical exports, especially syrups and liquid formulations. Each new contamination scandal threatens to tarnish India’s image as the “pharmacy of the world.”
Global agencies such as the World Health Organization have already called for stricter oversight and more transparent recall systems. If India hopes to maintain trust in its medicines abroad, experts say, it must demonstrate zero tolerance for quality lapses at home.
Public outrage over the deaths has reignited calls for comprehensive reform in India’s pharmaceutical sector. Experts have suggested several steps:
- Tighter Quality Testing: Every batch of pediatric syrups should undergo rigorous chemical analysis before reaching the market. Independent laboratories could be authorized to cross-verify samples.
- Accountability Mechanisms: Manufacturers, distributors, and even government inspectors should be held legally responsible for negligence leading to fatalities.
- Transparent Recall Systems: India lacks a nationwide platform for immediate product recall alerts. Such a system could save lives by removing harmful drugs quickly.
- Public Awareness: Parents should be educated about the dangers of self-medicating children with over-the-counter syrups. Pharmacists should also be trained to identify genuine products and report suspicious ones.
- Healthcare Infrastructure: Local hospitals must be equipped to handle poisoning emergencies. Dialysis centers and intensive care units should be available even in small towns.
The government’s decision to pursue criminal action represents an important shift. For the first time, there are signs that authorities may hold individuals accountable rather than allowing cases to fade from memory.
Still, accountability must extend beyond one company. Only when the entire supply chain — from ingredient sourcing to final packaging — is transparent and rigorously monitored can India ensure that tragedies like this never happen again.
The Coldrif case has laid bare the human cost of cutting corners in healthcare. For the parents who lost their children, no justice can bring them back. But for the country, this moment can serve as a reckoning — a chance to rebuild trust in the very system meant to protect its people.