New Delhi, 18 June 2025: Hepatitis, a viral infection that inflames the liver, is once again drawing nationwide attention in India as cases rise across several states. Often flying under the radar until complications become severe, This infections can progress silently in the body for months. With multiple variants, known as hepatitis A, B, C, D, and E, this disease presents a wide array of symptoms, risk factors, and modes of transmission. In light of recent outbreaks and rising hospitalization rates, particularly in Kerala and parts of northern India, public health experts are sounding the alarm on the urgent need for awareness, early detection, and timely treatment.
Understanding Hepatitis: What It Is and Why It Matters
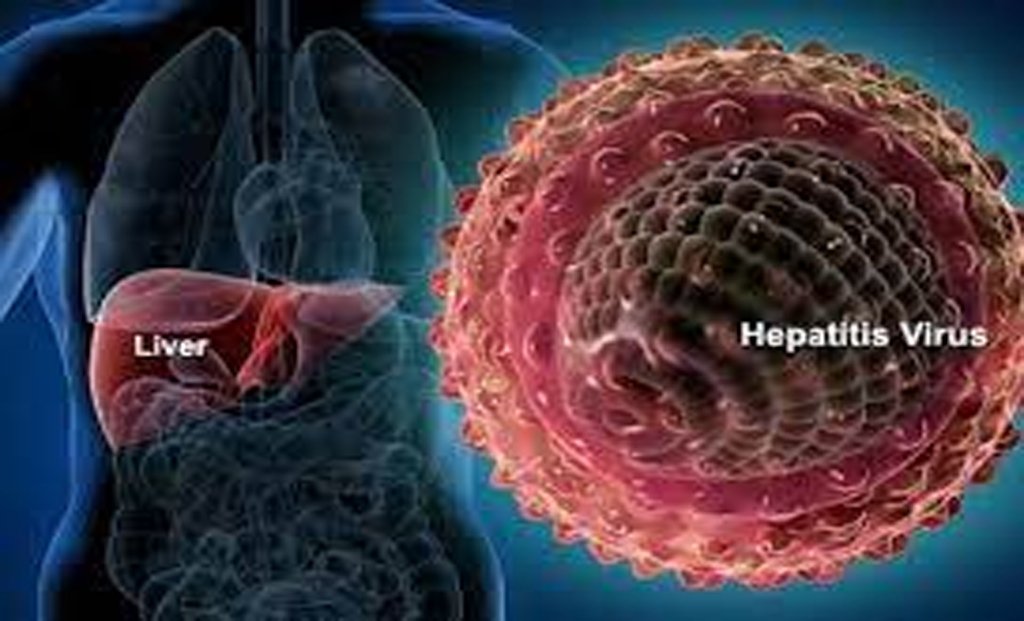
It refers to inflammation of the liver, most commonly caused by a viral infection. The liver is a critical organ responsible for filtering toxins, storing energy, aiding digestion, and producing vital proteins. When it becomes inflamed, its functions are impaired, leading to systemic consequences. This viruses, from A through E, vary in how they spread, how severe the illness becomes, and how long the infection lasts. Some forms of this resolve on their own with supportive care, while others may cause lifelong liver damage or cancer if left untreated.
Hepatitis A and E: Spread Through Contaminated Food and Water
This Disease A and E are typically transmitted through the fecal-oral route—often due to ingestion of contaminated food or water. These forms are more common in regions with poor sanitation and limited access to clean drinking water. Its A often affects children and young adults, while hepatitis E can be especially dangerous for pregnant women, sometimes leading to fatal liver failure. Symptoms include fatigue, nausea, vomiting, abdominal pain, dark urine, and jaundice, but many infected individuals show no symptoms, making community spread harder to detect. Although both types are acute and usually resolve on their own, they can occasionally cause severe liver dysfunction, particularly in vulnerable individuals.
Hepatitis B and C: The Silent Killers
Hepatitis B and C are more insidious forms of the disease. They spread primarily through contact with infected blood, unprotected sex, sharing needles, or from mother to child during childbirth. These variants are especially dangerous because they often remain asymptomatic for years, silently damaging the liver. Chronic hepatitis B and C infections can lead to cirrhosis (liver scarring), liver cancer, and ultimately liver failure if not treated in time. According to the World Health Organization (WHO), India is home to nearly 40 million people living with hepatitis B, and around 6–12 million people are estimated to have chronic hepatitis C, although many remain undiagnosed. Symptoms, when they do appear, are vague and include persistent fatigue, joint pain, mild fever, abdominal discomfort, and yellowing of the skin and eyes.
Hepatitis D: A Co-Infection that Worsens Outcomes
Hepatitis D is a peculiar virus that only infects individuals who already infected with hepatitis B. The co-infection worsens liver damage and accelerates disease progression, making early diagnosis and dual treatment essential. Though less common in India compared to other types, hepatitis D is dangerous because it increases the likelihood of fulminant hepatitis—a rare but deadly form of acute liver failure. Preventing hepatitis B through vaccination automatically lowers the risk of hepatitis D, emphasizing the importance of immunization programs.
The Silent Spread: Why Early Detection Is Crucial
One of the most alarming aspects of hepatitis is its capacity to spread unnoticed. Many individuals infected with hepatitis B or C experience no symptoms for years. The disease quietly progresses, damaging liver cells and eventually manifesting only when the damage is irreversible. This “silent” nature of It is what makes public awareness and regular screening so critical. At-risk populations—such as healthcare workers, intravenous drug users, people with multiple sexual partners, and those who receive frequent blood transfusions—should undergo regular testing. Simple blood tests can detect It markers early, allowing for timely intervention and management.
Prevention Through Vaccination, Hygiene, and Safe Practices
Vaccines are available for hepatitis A and B, and they offer a powerful defense against infection. The hepatitis B vaccine is part of India’s Universal Immunization Programme and recommended for all infants, with catch-up doses advised for unvaccinated adults. Hepatitis A vaccination is also available and especially important for travelers or individuals in outbreak-prone areas. For hepatitis C, there is no vaccine yet, but antiviral treatments have become highly effective in curing the infection if detected early. Personal hygiene practices like handwashing, boiling drinking water, avoiding street food in unsanitary conditions, and using condoms can significantly reduce the risk of hepatitis A, E, and B. Blood safety measures in hospitals and clinics, including screening of donors and use of sterile equipment, help control the spread of B and C.
India’s Ongoing Battle Against It
India faces a dual challenge: tackling active Its outbreaks while also managing the large burden of undiagnosed chronic cases. The Ministry of Health and Family Welfare has launched the National Viral Hepatitis Control Programme, which aims to eliminate hepatitis C by 2030, in line with WHO goals. Despite these efforts, lack of awareness, stigma, and inadequate access to testing and treatment facilities continue to hinder progress. Rural populations and economically disadvantaged communities disproportionately affected due to limited health literacy and infrastructure.
As It’s cases surge in parts of India, staying alert to the symptoms—even the subtle or silent ones—is more critical than ever. From the mild fatigue of early hepatitis A to the slow but relentless liver scarring caused by chronic hepatitis C, the disease spectrum is vast but preventable. Improved sanitation, vaccination drives, awareness campaigns, and regular screenings can together reduce the disease burden. At the personal level, adopting safe food and water habits, practicing protected sex, and getting vaccinated can go a long way in protecting individuals and their communities. As the nation navigates this is alert, knowledge and vigilance remain the most powerful tools against this often-overlooked viral threat.