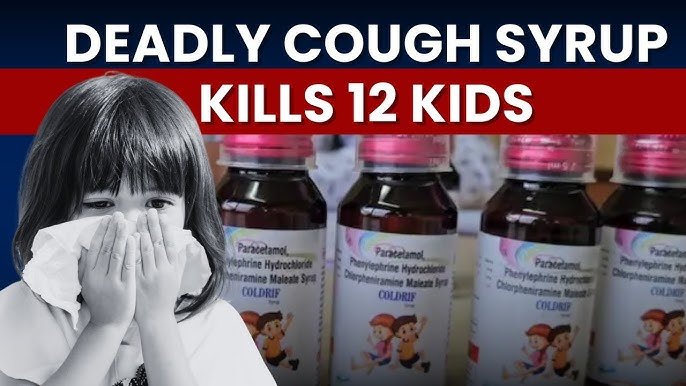
New Delhi, 19 October, 2025: In what may be one of the most disturbing medical scandals of recent years, authorities in India allege that a paediatrician received a 10% commission from a pharmaceutical firm for prescribing a cough syrup that has now been linked to the deaths of children. In one region of the country, at least 20 young children lost their lives after being given a cough medicine named “Coldrif”, which was later found to have been severely contaminated.
What Happened?
In one district, a doctor who was posted as a government paediatrician and also operated a private clinic, allegedly continued prescribing the syrup even after serious side‑effects began appearing in his patients. Investigators say he ignored governmental warnings against prescribing certain combinations of medicines to young children—even after noticing worsening kidney function in his patients.
According to the police case:
- The drug in question, Coldrif cough syrup, was later found to contain extremely high levels of a toxic chemical, far above safe limits.
- Children who consumed the syrup developed alarming symptoms: inability to urinate, elevated kidney markers (urea, creatinine), and acute kidney failure.
- Between August and October, multiple children under the age of five were treated with the syrup and later died or suffered irreversible damage.
- The doctor allegedly earned around Rs 2–8 per bottle prescribed—a 10% cut on the cost of the drug—despite the lives at stake.
Why This Is So Deeply Troubling
1. Breach of Trust
Parents bring their sick children to doctors believing they will get safe, effective treatment. To discover that the medication itself may have been dangerous—and that the doctor may have profited from prescribing it—is a profound betrayal.
2. Regulatory and Manufacturing Failure
The syrup’s contamination points to serious lapses in manufacturing quality control. A medicine meant to relieve children’s coughs instead caused kidney failure and death. The regulatory system failed to catch or act on the hazard until it was too late.
3. Conflict of Interest
Medical ethics demand that doctors make decisions in their patients’ best interests, free from undue influence. A commission‑based arrangement where a doctor receives payment for prescribing a particular drug creates a perverse incentive structure—putting profit above patient safety.
4. Vulnerable Population
The victims were among the youngest and most vulnerable—children under five, whose lives were cut short over what should have been minor ailments. Their passing raises serious questions about oversight, accountability, and the value placed on children’s lives.
What We Know So Far
- A doctor allegedly continued prescribing the syrup even after children under his care began suffering kidney damage.
- The commission was around 10% of the cost of each bottle. In one report, the doctor received Rs 2.54 for each bottle priced at Rs 24.54.
- The manufacturer has been shuttered, key personnel have been arrested, and investigations into the supply chain—including wholesaler licences and storage practices—are ongoing.
- Children died after symptoms of kidney failure, in spite of treatment. Many had been administered the syrup for what started as common cough or cold.
What Led to This Tragedy?
A chain of errors and misdeeds appears to have converged:
- A syrup formulation that should have been safe was contaminated with a toxic solvent.
- A doctor who allegedly ignored early warning signs and continued prescribing the drug—possibly influenced by financial incentive.
- Weak regulatory enforcement and unchecked distribution of the drug to children under recommended ages.
- A supply and prescription system where profit, not patient welfare, became a factor in medicine choice.
Who Is Responsible?
Multiple actors share responsibility:
- The Manufacturer: For producing or distributing a toxic batch of medicine and failing in quality control.
- The Distributing Chain: Wholesalers, stockists, and pharmacies who continued to supply the drug despite red flags.
- The Prescribing Doctor: For continuing to administer the syrup in the face of warnings and possible benefit from commissions.
- Regulators and Oversight Agencies: For failing to catch the contamination earlier and preventing unsafe prescription practices.
What Happens Next?
- Full judicial and police investigations are underway.
- The manufacturing licence of the company has been cancelled.
- Authorities are tracing the distribution chain to identify how such dangerous syrup reached children.
- Claims for accountability from all levels of the system—from doctor to factory owner to regulator—are being pursued.
- Parents and communities are demanding justice and reforms to ensure no child is subjected to medicine that harms rather than heals.
How This Impacts You and Your Loved Ones
- Always check medicine origin, batch number, and approval status, especially for children.
- Ask questions about prescription motives: Is this drug the only option? Could a safer alternative be used?
- Ensure the doctor you trust is transparent and doesn’t have hidden incentives. A prescription should be made based purely on medical necessity, not manufacturer influence.
- For parents: Monitor children closely after giving any medicine, especially if it is a cough syrup or combination drug for very young children. Early signs of kidney distress (reduced urination, swelling, fatigue) require urgency.
- Advocate for stricter regulation, transparency in pharmaceutical practices, and accountability in healthcare prescribing norms.
The loss of so many children over what began as simple coughs is a tragedy of monumental proportions. At its heart it is a story about trust betrayed, systems failed, and the value of children’s lives that were sacrificed—supposedly for a mere few rupees per bottle.
If any positive can come from this horror, it must be a reckoning: that medicine must be safe and prescribing must be ethical. That doctors must keep profit out of the consulting room. That manufacturers must adhere to the highest standards. And that society must demand better oversight, especially when it comes to the youngest among us.
Because every child’s life counts. And in this case, the cost of negligence was far greater than any bottle of syrup ever should have been.