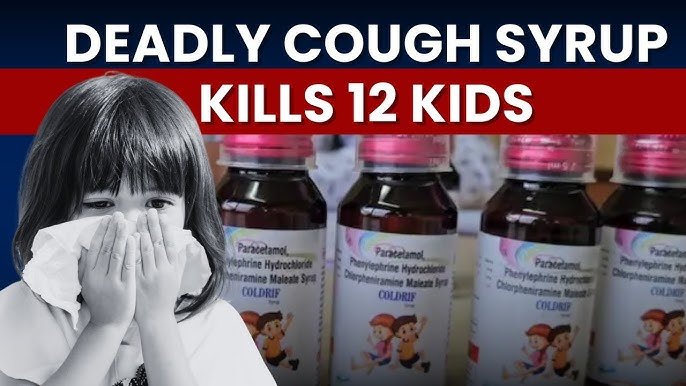
New Delhi, 05 October, 2025: The state of Madhya Pradesh has been shaken by a tragic incident involving Coldrif cough syrup, which has been banned after at least 11 deaths were linked to its consumption. The deaths, reported primarily from Ujjain district, have raised alarm across India about drug safety, manufacturing oversight, and the recurring issue of contaminated syrups — a problem that has already claimed lives in several other countries.
According to health authorities, samples of Coldrif cough syrup were found to contain a toxic solvent, suspected to be diethylene glycol (DEG) or ethylene glycol (EG) — chemicals known for their deadly effects on the kidneys and nervous system. Two doctors from the local hospital have been arrested for allegedly prescribing and distributing the syrup without proper verification, as investigations continue into the source of contamination.
The Tragedy in Ujjain: How It Unfolded
The alarm was first raised when several patients, including children, presented at hospitals in Ujjain and surrounding areas with symptoms of poisoning, such as nausea, vomiting, abdominal pain, and decreased urine output. Within days, multiple deaths were reported, all linked by one common factor — the use of Coldrif cough syrup.
Preliminary investigation revealed that the syrup was manufactured by a local pharmaceutical company and distributed across parts of Madhya Pradesh. The state health department immediately ordered seizure of remaining stocks, followed by a complete ban on its sale and distribution.
Officials from the Central Drugs Standard Control Organisation (CDSCO) and Food and Drug Administration (FDA) are now conducting laboratory tests to confirm the exact nature and quantity of the toxic substance present in the samples. Early reports indicate that the solvent used in the formulation was not pharmaceutical-grade, which led to contamination.
What Made the Syrup Deadly: The Toxic Solvent Link
The most alarming finding in the investigation so far is the presence of industrial-grade diethylene glycol (DEG) or ethylene glycol (EG) — substances that are commonly used in antifreeze and brake fluid, not in medicines.
These toxic chemicals are sometimes used as cheaper substitutes for glycerin or propylene glycol — safe solvents that help dissolve active ingredients in syrups. When pharmaceutical manufacturers cut corners or procure ingredients from unregulated suppliers, such substitutions can have catastrophic health effects.
How DEG and EG Affect the Body
- Kidney Damage: Both DEG and EG are metabolized into toxic compounds that severely damage the kidneys, often leading to acute renal failure.
- Neurological Symptoms: Patients may experience confusion, seizures, and coma as the toxins affect the central nervous system.
- Metabolic Acidosis: The body’s pH balance drops sharply, leading to organ dysfunction and potentially death if untreated.
Medical experts emphasize that even small amounts of these chemicals can be fatal, particularly for children and elderly patients.
Recurring Problem: A Global Pattern of Contaminated Cough Syrups
The Coldrif case is not an isolated incident. Over the past few years, India’s pharmaceutical exports have faced international scrutiny following several deadly outbreaks linked to contaminated cough syrups in The Gambia, Uzbekistan, and Cameroon.
In each of those cases, DEG or EG contamination was found to be the cause of acute kidney failure in children.
India, one of the world’s largest drug manufacturers, exports medicines to over 200 countries. While the majority of its pharmaceutical production meets global standards, a few small or unlicensed manufacturers continue to operate with poor quality controls and unregulated sourcing practices, tarnishing the country’s reputation and endangering lives.
Experts Warn: Stronger Oversight and Testing Needed
According to senior pharmacologists and toxicologists, the tragedy underscores the urgent need for stricter surveillance across the entire pharmaceutical supply chain — from raw materials to final distribution.
Dr. R.K. Sharma, a pharmacovigilance expert, explained,
“This is not just about one bad batch. It’s about systemic lapses — poor quality checks, lack of routine testing, and unchecked local manufacturing. Every bottle of medicine that reaches a patient must undergo verified safety testing.”
The Health Ministry has reportedly instructed all state-level drug controllers to review cough syrup samples currently in circulation and ensure compliance with Good Manufacturing Practices (GMP).
Experts recommend random batch testing and traceability systems that can quickly identify and recall contaminated products before they cause harm.
What Consumers Should Know: Recognising the Risks
Public health experts are urging people to exercise caution while buying over-the-counter syrups, especially in rural or small-town pharmacies.
Here are some key safety tips to keep in mind:
- Check the Manufacturer’s Details: Always verify that the product is from a licensed, recognized brand.
- Avoid Unlabeled or Unsealed Products: Counterfeit or refilled bottles are common in unregulated markets.
- Be Wary of Unusual Taste or Odor: Toxic syrups may have a strong chemical smell or taste.
- Avoid Self-Medication: Always consult a doctor, especially for children or long-term cough symptoms.
- Report Adverse Effects: If someone experiences vomiting, dizziness, or reduced urine output after taking a syrup, seek emergency care immediately and report the case to local health authorities.
The Legal and Ethical Fallout
Following the Ujjain deaths, the Madhya Pradesh government ordered a state-wide crackdown on pharmaceutical companies suspected of violating quality norms.
Two doctors at a local hospital were also arrested under charges of negligence and culpable homicide, as they allegedly continued to prescribe and administer the syrup even after initial warning signs appeared.
Authorities are also investigating whether the raw materials were procured illegally from unlicensed suppliers. If confirmed, it could lead to broader criminal charges under India’s Drugs and Cosmetics Act, 1940.
The state has also announced compensation for the victims’ families and assured the public that corrective measures are being implemented to prevent similar incidents.
A Call for Change: Prioritising Drug Safety in India
The Coldrif tragedy has reignited national debate over pharmaceutical regulation in India. Experts are calling for:
- Regular third-party audits of small and medium drug manufacturers.
- Mandatory testing of solvent quality before approval.
- Public transparency reports on drug recalls and safety violations.
- Harsher penalties for companies found guilty of adulteration or negligence.
Public health advocate Dr. Meenakshi Das said, “Every death due to a preventable cause like this is a policy failure. India needs to treat drug safety with the same seriousness as food or air safety — because the consequences are just as deadly.”
A Wake-Up Call for India’s Healthcare System
The Coldrif cough syrup deaths in Madhya Pradesh are a grim reminder that patient safety cannot be compromised. While the investigation continues, the incident has already exposed critical flaws in India’s drug manufacturing and monitoring system.
As World Health Organization guidelines reiterate, every cough syrup batch should be tested for toxic solvents before release. The tragedy underscores the importance of regulatory vigilance, accountability, and responsible medical practice.
For now, health authorities are urging citizens to remain alert and avoid unverified medicines. But the long-term solution lies in building a stronger, transparent, and ethically driven pharmaceutical ecosystem that puts human life above profit.